Bioequivalence of narrow therapeutic index drugs and immunosuppressives
Published on 2015/11/19
Generics and Biosimilars Initiative Journal (GaBI Journal). 2015;4(4):159-60.
Author byline as per print journal: Christoph Baumgärtel, MD, MSc; Brian Godman, BSc, PhD
|
Abstract: |
Submitted: 29 September 2015; Revised: 19 October 2015; Accepted: 19 October 2015; Published online first: 2 November 2015
Regulatory bioequivalence rules for usual generics are well established and already recognized. However, for narrow therapeutic index drugs and immunosuppressives, there are specific and tighter criteria in place.
Drugs with a narrow therapeutic index are defined by a narrow distance between the dosage that induces a desired effect and that dosage which already has a toxic effect. Typically, this ratio in the field of pharmacology is indicated by the quotient of LD50/ED50 (LD50 = the dose at which 50% of the animals die, ED50 = the dose at which 50% of the animals show the desired effect). Alternatively, the quotient of LD5/ED95 can be used, which can better illustrate a non-linear dose-response curve.
For a perfectly safe drug, the ratio should therefore be very high. If in contrast the ratio is low, i.e. if a drug shows a value of only 3 or 4, this is called a ‘narrow therapeutic index drug’ (NTI), which must always be dosed with particularly high accuracy. Even a minor variation in plasma levels may lead sometimes to treatment failure on the one hand or inevitably to toxic effects on the other. Examples of such agents typically include immunosuppressants, digitalis, theophylline and some anti-epileptic drugs.
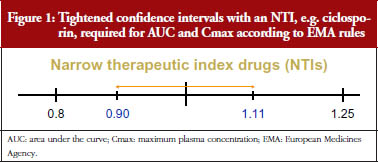
The acceptance range of bioequivalence trials which is usually applied for a marketing authorization of a generic drug is 80–125% of the 90% confidence interval of the ratio of the test and reference products’ AUC (area under the curve) and Cmax (maximum plasma concentration). For drugs with a narrow therapeutic index, and especially for immunosuppressives, the European Medicines Agency (EMA) demands even greater accuracy in justified cases and therefore has set more stringent criteria. This is despite in practice ratios for authorized conventional generics usually differ on average by only three to four per cent from their originator [1–4].
EMA’s overhauled bioequivalence guideline [5], in force since 2010, requires that for potential narrow therapeutic index drugs the EMA’s Pharmacokinetic Working Party (PKWP) [6] will evaluate if a generic drug newly submitted for authorization is to be thought of as an NTI and whether for this NTI actually stricter bioequivalence criteria have to be applied. It is important for a pharmaceutical manufacturer or applicant to know that there is no precasted list that names all such agents, but that all agents submitted for generic drug authorization will be evaluated by the authority on a case-by-case basis with regard to their NTI requirements.
Examples where this has already been practised are the regulatory requirements for ciclosporin and tacrolimus generics as described in a PKWP Questions and Answers document published on the EMA website [7]. In the case of these two immunosupressives, restricted bioequivalence criteria were set.
For ciclosporin, narrower acceptance intervals of 90.00–111.11% are required for both the AUC and the Cmax. Whereas, for tacrolimus the narrow acceptance interval is only required for the AUC but is not required for the Cmax. This is because tacrolimus plasma levels show accumulation with repeated dosing, resulting in a lower relevance being given to differences in initial peak plasma concentrations..
The narrower acceptance range limits for the confidence intervals for NTIs, see Figure 1, provide a greater confidence in the true bioequivalence for these drug substances. However, this requirement significantly increases the number of subjects necessary for the bioequivalence studies. Tacrolimus, for example, is a drug which is not merely an NTI, but additionally shows relatively high intra-individual variation in plasma levels. It has a relatively high coefficient of variation, close to 30%, which would classify it as a highly variable drug. Even in bioequivalence trials of tacrolimus, when a conventional acceptance range is applied, this would typically necessitate enrolling substantially higher numbers of trial participants than in the usual, bioequivalence guideline requiring a minimum of 12 to 24 subjects. One would need at least 40 subjects for a tacrolimus product, and in fact to demonstrate compliance with EMA’s mandatorily required narrower acceptance limits, it might require up to 200 to 300 subjects.
To increase the safety of generic immunosuppressives even more, it is also recommended that the summary of product characteristics (SPC) states that patients who are prescribed either a generic immunosuppressant after an originator or are switched in any other way, have their plasma levels monitored during the time of the switch to avoid potential rejection [8]. This is however similar to what is undertaken in normal clinical practice when patients are first placed on an immunosuppressant after receiving a solid organ graft.
Because of the issues concerning generic immunosuppressive medicines, Molnar et al. recently undertook a systematic review and meta-analysis of all available studies since 1980 comparing generic with originator (innovator) immunosuppressive medicines [9]. The authors documented that acute rejection was rare in transplant patients given generic immunosuppressive medicines and the incidence of rejection did not differ between the groups. However, as recently stated, the methodological standard of the published studies included was very variable and follow-up times were short [10].
In the evaluation of the pooled pharmacokinetic data, Molnar et al. showed that the generics met the US Food and Drug Administration (FDA) bioequivalence criteria, but did not all meet the stricter EMA criteria [9]. It appears that the small number of patients in some of the included studies, and as a result the wide confidence intervals, significantly contributed to this finding. For statistical reasons, in order for results to meet the stricter acceptance criteria for immunosuppressives, requiring narrow confidence intervals, a sufficiently higher number of patients must be included in the trials [11].
This effect on subject numbers needed is illustrated by the wide confidence intervals found in immunosuppressive studies with less than 20 subjects. As reviewed in the paper by Molnar et al., only trials with approximately 50 to 70 patients were able to fulfil the EMA acceptance criteria [9]. In detail, their sub-analysis of two randomized kidney trials showed that with a mean of 30 subjects, both failed to fulfil the stricter EMA bioequivalence criteria, whereas the pooled sub-analysis of seven non-randomized interventional kidney studies with a 53% higher mean sample size of 46 patients did fulfil these criteria.
Notably, the mean ratios of the test and reference products’ AUC and Cmax in most of the reported trials were well within the expected range [12]; and were in fact only a few percentage points higher or lower than 100% [9]. These data strongly suggest that there are no clinically important problems with generic immunosuppressive agents, especially with those that meet the EMA criteria, but rather that there are problems with the scientific value, relevance and interpretation of smaller studies.
It should also be noted that EMA’s precautious narrowing of bioequivalence limits was specifically implemented for situations where it is suspected that plasma level monitoring will – against the SPC advice – not be complied with; such as following a switch from an originator to a generic drug [7]. This narrowing can therefore be seen as a ‘safety net’ for the use of immunosuppressive generics. This suggests that generic immunosuppressive drugs, used in the correct manner by practitioners aware of their precautions, especially the requirement for monitoring of plasma levels at the time of switching, may indeed be considered to be bioequivalent and expected to produce outcomes that are similar to those produced by originator products.
This expectation is supported by the fact that generic versions of immunosuppressive medicines, i.e. ciclosporin, have been on the market in Europe for more than 10 years and authorities’ pharmacovigilance systems have not identified any serious issues specific for generic immunosuppressives, even after an estimated hundreds of thousands of prescribed and dispensed doses. This should alleviate major concerns among clinicians and patients when considering or undertaking a switch. However, it is expected that further well-designed studies with a suitable number of patients will help to fully address any remaining concerns with generic immunosuppressives. Further education among physicians about the need to reliably moni tor blood levels in patients when first prescribed generic immunosuppressives will also be needed. Such activities may also help to enhance adherence to immunosuppressive medicines, which is a crucial concern in transplant patients [13].
Competing interest: None.
Provenance and peer review: Not Commissioned; externally peer reviewed.
Co-author
Christoph Baumgärtel, MD, MSc, Senior Scientific Expert, Coordination Point to Head of Agency, AGES Austrian Medicines and Medical Devices Agency and Austrian Federal Office for Safety in Health Care, EMA European Expert, Vice Chair of Austrian Prescription Commission, 5 Traisengasse, AT-1200 Vienna, Austria
References
1. American Medical Association. Featured report: generic drugs (A-02), June 2002 AMA Annual Meeting [homepage on the Internet]. [cited 2015 Oct 19]. Available from: http://www.ama-assn.org/ama/pub/about-ama/our-people/ama-councils/council-science-public-health/reports.page?
2. Henney JE. From the Food and Drug Administration. JAMA. 1999;282(21):1995
3. Nwakama PE. Generic drug products demonstrate small differences in bioavailability relative to brand name counterparts: Review of approved ANDAs, FDA. 2015
4. Davit BM, et al. Comparing generic and innovator drugs: a review of 12 years of bioequivalence data from the United States Food and Drug Administration. Ann Pharmacother. 2009;43(10):1583-97.
5. European Medicines Agency. Committee for Medicinal Products for Human Use (CHMP). Guideline on the investigation on bioequivalence. EMA: CPMP/EWP/QWP/1401/98 Rev. 1. January 2010 [homepage on the Internet]. 2010 Mar 10 [cited 2015 Oct 19]. Available from: http://www.ema.europa.eu/docs/en_GB/document_library/Scientific_guideline/2010/01/WC500070039.pdf
6. European Medicines Agency. Pharmacokinetics Working Party [homepage on the Internet]. [cited 2015 Oct 19]. Available from: http://www.ema.europa.eu/ema/index.jsp?curl=pages/contacts/CHMP/people_listing_000070.jsp&mid=WC0b01ac05802327c9
7. European Medicines Agency. Committee for Medicinal Products for Human Use (CHMP). Questions & answers: postitions on specific questions addressed to the Pharmacokinetics Working Party (PKWP). EMA/618604/2008 Rev. 12. 25 June 2015 [homepage on the Internet]. 2015 Jul 20 [cited 2015 Oct 19]. Available from: http://www.ema.europa.eu/docs/en_GB/document_library/Scientific_guideline/2009/09/WC500002963.pdf
8. Austrian Federal Office for Safety in Health Care. Austrian Medicines and Medical Devices Agency. Available from [homepage on the Internet]. [cited 2015 Oct 19]. Available from: https://aspregister.basg.gv.at/aspregister/
9. Molnar AO, et al. Generic immunosuppression and solid organ transplantation: systematic review and meta-analysis. BMJ. 2015;350:h3163.
10. Godman B, Baumgärtel C. Are generic immunosuppressants safe and effective? BMJ. 2015;350:h3248.
11. Baumgärtel C. [Bioequivalence – narrow therapeutic index drugs]. Bioäquivalenz – Arzneimittel mit enger therapeutischer Breite. ÖAZ, Österreichische Apotheker Zeitung. 2012;66(23):60-1. German.
12. Baumgärtel C. Myths, questions, facts about generic drugs in the EU. Generics and Biosimilars Initiative Journal (GaBI Journal). 2012;1(1):34-8. doi:10.5639/gabij.2012.0101.009
13. Tong A, Howell M, Wong G, Webster AC, Howard K, Craig JC. The perspectives of kidney transplant recipients on medicine taking: a systematic review of qualitative studies. Nephrol Dial Transplant. 2011;26(1):344-54.
|
Author for correspondence: Brian Godman, BSc, PhD, Division of Clinical Pharmacology, Karolinska Institutet, Karolinska University Hospital Huddinge, SE-14186 Stockholm, Sweden |
Disclosure of Conflict of Interest Statement is available upon request.
Copyright © 2015 Pro Pharma Communications International
Permission granted to reproduce for personal and non-commercial use only. All other reproduction, copy or reprinting of all or part of any ‘Content’ found on this website is strictly prohibited without the prior consent of the publisher. Contact the publisher to obtain permission before redistributing.